 They’re microscopic insects crawling around your skin pores, perfectly adapted to human skin.
They’re microscopic insects crawling around your skin pores, perfectly adapted to human skin.
They’re the real root cause of acne that every teenager has been searching for, according to internet posters.
5 years ago, we concluded that demodex mites almost certainly aren’t causing your acne, but could add additional fuel to the inflammation fire.
Has anything changed since then? What’s certain is that numerous new studies have been unleashed upon the world, and here’s what they say…
The story so far
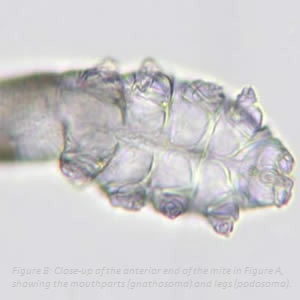
As covered in 2015, demodex mites are 0.3 to 0.4mm long insects which commonly reside on human skin.
They normally don’t bother us, and go about their activities harmlessly, but become more common after age 25, essentially as you brush against more and more passersby, whether in airports or taxis. They’re semi transparent insects, although unfortunately, they don’t glow in the dark.
A demodex mite lives a fast and hard life. It hatches from an egg, becomes an adult on day 6, becomes a father on day 7 (presumably), and dies a fulfilled mite in an explosion of protein on day 14.
Demodex mites certainly capture the imagination; most people leap back with revulsion at the thought of crocodile-like insects crawling, sleeping and even having sex all over your skin. The wild root cause theories aren’t surprising – it all seems to click into place when you first stumble across them. That’s why all the cleansers I’ve tried failed, people think.
However, it’s a known fact that demodex mites stimulate inflammation. Unlike acne, they’re essentially proven to cause rosacea, the red skinned imposter acne caused by a haywire immune system.
There are too many fantastic testimonials of anti-demodex medications like permethrin, total revolutions, for us to ignore. Their death supposedly clogs your pores as they tumble backwards into them, which is unproven, but has a glimmer of potential given that the skin pores are their main hidey-holes.
Nevertheless, the bottom line in 2015 was that no acne studies existed showing uncontrollable infestations – just mildly increased levels. So here’s the official 2020 update…
Have demodex mites been unmasked?
 Firstly, we’ll start with a 2018 study that could be revolutionary. Quite simply, it found that 62.4% of acne patients had a demodex infestation versus 16.7% of controls, as defined by 5 or more mites per square centimetre of skin.
Firstly, we’ll start with a 2018 study that could be revolutionary. Quite simply, it found that 62.4% of acne patients had a demodex infestation versus 16.7% of controls, as defined by 5 or more mites per square centimetre of skin.
A teenager might see this figure floating around the internet and think that he’s finally find the cure. The reliable was undeniable: there were 210 acne patients, a strong number to avoid anomalies, and 150 clear-skinned controls.
Their left cheeks, right cheeks, nasolabial area (where smiling lines appear) and chin were all sampled, because it’s always possible that one tiny area like the chin is infected, but others aren’t. Each area was tested twice.
Women had higher densities of demodex mites, but men had higher rates of infection. Whether this is significant is a mystery, but the severity of acne was also important. Severe patients (45 people) had 117.1 mites per cm2, moderate had 43.5, while mild had only 21.0. It was an extremely tight correlation.
If this was the only fresh study since 2015, then demodex mites would officially be on our acne radar.
But the storm clouds gathered with this deceptive 2018 experiment. Demodex mites had tighter connections to acne than alcohol and smoking, which is saying something. Officially, 42.6% of 108 acne patients were infected versus 12.3% of the 65 clear-skinned controls. Adolescents were particularly striking: 44.6% infestation versus 0% of the controls. In adults, it was 39.6% versus 21.1%.
It was a similar concept to the previous study, and an equally fantastic result…
Yet one mistake scuppered everything. The scientists only chose volunteers with known oily skin.
Like acne bacteria, demodex mites feed off human sebum to live, digesting its fats to go about their day, despite only having 14 of them. Oily people are inherently more likely to be infected, and therefore, this study cuts out a huge chunk of real life acne patients. Acne patients with dryer skin, but countless tiny, red, angry pimples, might have no link to demodex mites.
There’s another crack in the armour too: 42.6% is 3 times bigger than 12.3%, but it clearly rules out demodex mites being the secret root cause. Not even half of patients were infected. That’s before we consider how damaging those mites actually are.
It’s the most eye catching study on the list, but it also has the most crippling methodological flaw.
Study 1 effectively stands alone, and as you’ll soon see, it is gravely outnumbered…
A resoundingly negative study
Interestingly, not one study has found an inverse relationship, e.g. acne patients with dramatically lower infection rates than controls. However, this 2016 experiment did find no correlation whatsoever.
The main goal was testing a new demodex mite detection method, but as usual, the secondary result was way more interesting. This happens constantly; a classic example is scientists’ obsession with using nanoparticles to enhance antibacterial remedies. You glance at the study, and then your head spins around and you say “hang on!”: since when was tamanu oil proven to kill p.acnes?
Anyway, this is our most negative study: unlike rosacea, demodex mites were no higher whatsoever in acne sufferers. Seborrhoeic dermatitis and atopic dermatitis were also no different. Meanwhile, only 3/215 rosacea patients had normal demodex mite levels, which is even more extreme than usual.
Reliability-wise, some believe that the normal film placed on the face and ripped off after one minute is too shallow, skipping demodex mites lurking deeper in the pores, particularly d.brevis. However, this study used a revolutionary new system, and it still didn’t find huge differences. It might have captured more mites in the control and in the acne patients. Regardless, it piles on the reliability points.
The acne patients numbered only 47, despite the study containing 1046 people. However, it’s a fairly reliable study overall and not fatally flawed like number 2.
4-6: the same old story
 So far then, it’s one positive study, one negative, and one house of cards which collapsed under the slightest examination.
So far then, it’s one positive study, one negative, and one house of cards which collapsed under the slightest examination.
The next three reinforce our old stance to the letter. It’s mildly important for acne, but pales compared to rosacea…
FOUR: in this battle royale we have 43 acne patients, 43 for team rosacea, and 41 with seborrhoeic dermatitis. Compared to the 77 clear-skinned people, 52% of the rosacea patients were demodex positive versus just 2.6%. Acne was “significantly associated” with these invisible bugs, but nevertheless, infestation rates were far lower than rosacea.
Reliability-wise, a dermatologist counted the pimples rather than an infallible machine. However, it was always the same dermatologist, giving it some equality, making the subjective opinions the same. The scientists also excluded “complicated variants” of acne like the horrific, burrowing acne conglobota. They tested the acne we all know and love, or loathe.
There’s one serious flaw: the rosacea group was easily the oldest, and demodex mite infestation is proven to increase with age. Likewise, the acne group averaged at the youngest. This was purely a mistake and not intentional. They also used shallow sampling paper that might have missed the deepest mites. Verdict: informative, but not cast iron.
FIVE: the overview here appears very negative, saying “There is no relationship between Demodex and acne lesions number“. However, scouring the raw data revealed that 42.4% of acne patients tested positive compared to 11.9% of controls. Take note: these numbers are fascinatingly similar to study 2. Once again, the false acne called papulopustular rosacea (more here) had 90.2% infection, with a demodex density of 36 per cm. For acne and healthy skin, the densities were 1.77 and 0.7 respectively.
The reason for the pessimistic verdict? When the patients were bathed in a demodex killing cleanser, their acne failed to improve whatsoever. The infestations might have been purely coincidental, but here, there’s a fatal flaw: the cleanser experiment lasted just 7 days. That’s nowhere near enough time to soothe inflammation – the bugs might have collapsed and died (or leapt from their faces heroically) on only the 6th day. The first experiment was reliable, however, with a sizeable 132 acne patients.
SIX: a nice, basic study where demodex infection was measured yet again, from the swabbed skin samples of human beings.
In their words: “demodex was detected more frequently in patients with rosacea than… acne“. However, there was a still a decent link, at 56.5% versus 45.9%. Patients with stage 1 demodecosis, when the skin is so infested that it graduates to a clinical disease, were much more likely to have stage III or IV acne, as defined by the American Academy Of Dermatology (rather than ones they randomly invented).
The mites were taken from all over the face, from the cheeks, forehead, chin and nose. The reliability was strong, with 44 men and 106 women with a mean age of 29.6. They even banned pregnant women, lactating women, drug addicts and alcoholics from the study.
Three studies, and three verdicts that demodex mites are connected to acne, but nowhere near as tightly as rosacea.
If you have rosacea, on the other hand, then the time is now! You’ve hit the jackpot.
Number 7 – only important for severe acne
That’s the verdict of our final study (2019), which gathered a neat 30 healthy patients, 30 severe acne patients and 30 mild/moderate.
The infestation was 6.7% for clear-skinned controls. This fell to 0.0% for mild acne, before leaping to 40% for severe acne. The stone cold 0% was probably statistical noise, but the jump can’t be ignored: “Our result found an association between acne vulgaris and Demodex infestation“.
As a bonus, poor use of cleansers, sun exposure, stress, being a man, and oily skin were also linked to mite infestation.
It’s very possible that demodex mites are irrelevant with the occasional mild pimple, but explain why some people’s acne gets to extreme levels where your face is barely recognisable. Study 2 was similar, with 117.1 mites per cm2 in severe acne and 21.0% in mild.
It fits with our concept not being the root cause, but instead piling the inflammatory fuel on the fire. The rate was only 40%, which strangely, matches studies 2, 5 and 6 closely.
Demodex mites could explain why some people’s acne stubbornly refuses to heal. Honey would do nothing; they would probably lick it up. However, tea tree oil does kill the mites, possible explaining why some topical treatments randomly cause miracles while others fall flat. There are many variables in this demodex equation.
Analysis time
Essentially, our existing theory has solidified like magma.
The chances that demodex mites are mostly a supporting character have risen, leaving open room for occasional people where demodex madness is the real cause. Demodex mites still aren’t the secret supervillains pulling the strings of everybody’s acne woe – that smiling jar of soybean oil is the real troublemaker.
As you stare at the computer screen, your demodex mite families/colonies might be reading this article too, nodding their heads in agreement, with popcorn in hand.
Here’s the official lowdown. We have two grand studies of demodex doom, one highly reliable, and one which disintegrates with the slightest touch. We have one reliable study exonerating demodex mites totally.
Then we have 4 imperfect, but mostly reliable experiments saying that acne patients have more demodex mites, but not compared to rosacea patients. The two outlier studies can’t be ignored, but our theory is still on the rails.
There’s one question remaining – could acne and demodex mites be two branches of the same tree?
Specifically, could they both be caused by oily skin, an environmental favourable to both, rather than having any real connection? We pondered this last time, but today’s studies give us no clarity. It’s a real possibility, or it could be 50/50, with a small chunk being genuine inflammation from the mites.
There’s only one way we’ll find out: by testing a demodex-killing cream with no effect on oily skin, in an 8 week experiment.
A mystery: the different types of demodex
Another uncharted land of the demodex universe is the 65 different subspecies.
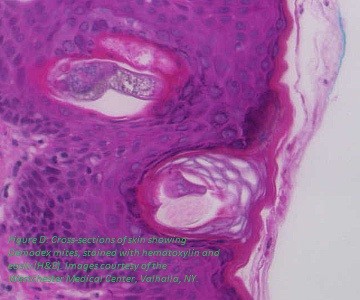
Only demodex folliculorum and demodex brevis live on human skin. D. folliculorum roam the outer skin pores, and shallow areas of the hair follicles. It’s the “main” demodex as it was discovered in 1842, versus 1963 for D.brevis. These guys are shier, and hide in the deep structures of the skin, even inside the sebaceous glands themselves.
According to study seven, d.folliculorum has an “energetic lifestyle” while d.brevis has a “lethargic lifestyle”, which they undoubtedly wrote with a disapproving shake of the head.
They’re the bowling-loving stoners of the demodex kingdom, darting around much less under a microscope. Physically, d.folliculorum is long while d.brevis is short.
Interestingly, nobody has a clue which species, if either, is worse for acne. The method is the demodex mite’s spectacular deathstyle, falling sick before exploding into a messy mass of inflammatory proteins. It’s possible that the proteinaceous goop has subtle differences between species, but we have no idea…
…and this leads to the classic problem. Because d.brevis is like that subterranean race of human beings which we’re supposedly destined to discover, lurking in underground tunnels where the sun never shines, could the experiments be missing them?
The standard SSSB method cannot reach deeply into pores, by the scientists’ own confession. This involves placing a film on the face for 1 minute, to capture outer skin cells and sebum (oil). It’s perfect for kidnapping the marathon runners of d.folliculorum, scurrying around on the surface (which is probably like the Great Plains of Wyoming to them).
For example, if d.brevis is worse, then the studies showing only moderate correlations with acne might be limited in vision. D. brevis might be busy triggering the immune system in its underground caves, without scientists knowing.
If d.folliculorum infestations triple in acne patients (from 12% to 40%, for example), d.brevis could secretly rise by 10-fold. However, this applies both ways: healthy people’s colonies could also be underestimated.
In study 6, the ratio tilted towards d.folliculorum the more severe the acne got. It sounds informative at first, but they still used the shallow scraping method: d.brevis could have been swarming beneath the surface.
The role of different species is equally mysterious to whether demodex mites cause acne in the first place.
Conclusion
The verdict is unchanged – demodex mites may contribute to acne, but probably aren’t causing it.
The secret recipe for clear skin is actually vitamin E mixed with pomegranate seeds sprinkled with zinc shards.
We have one last bonus fact: in study two, alcohol consumption was strongly linked to demodex mite infestation, particularly after age 25.
Why is a mystery, but immune system alterations are a possibility. Alcohol increases the fatty acid ethyl esters in your skin’s oil, and perhaps it makes their energy source even more delicious for them.
Thanks for reading!